As many of our clients and friends know, our Production Manager Rob and Wife Kim have an amazing Son Jude who was born with a heart defect.
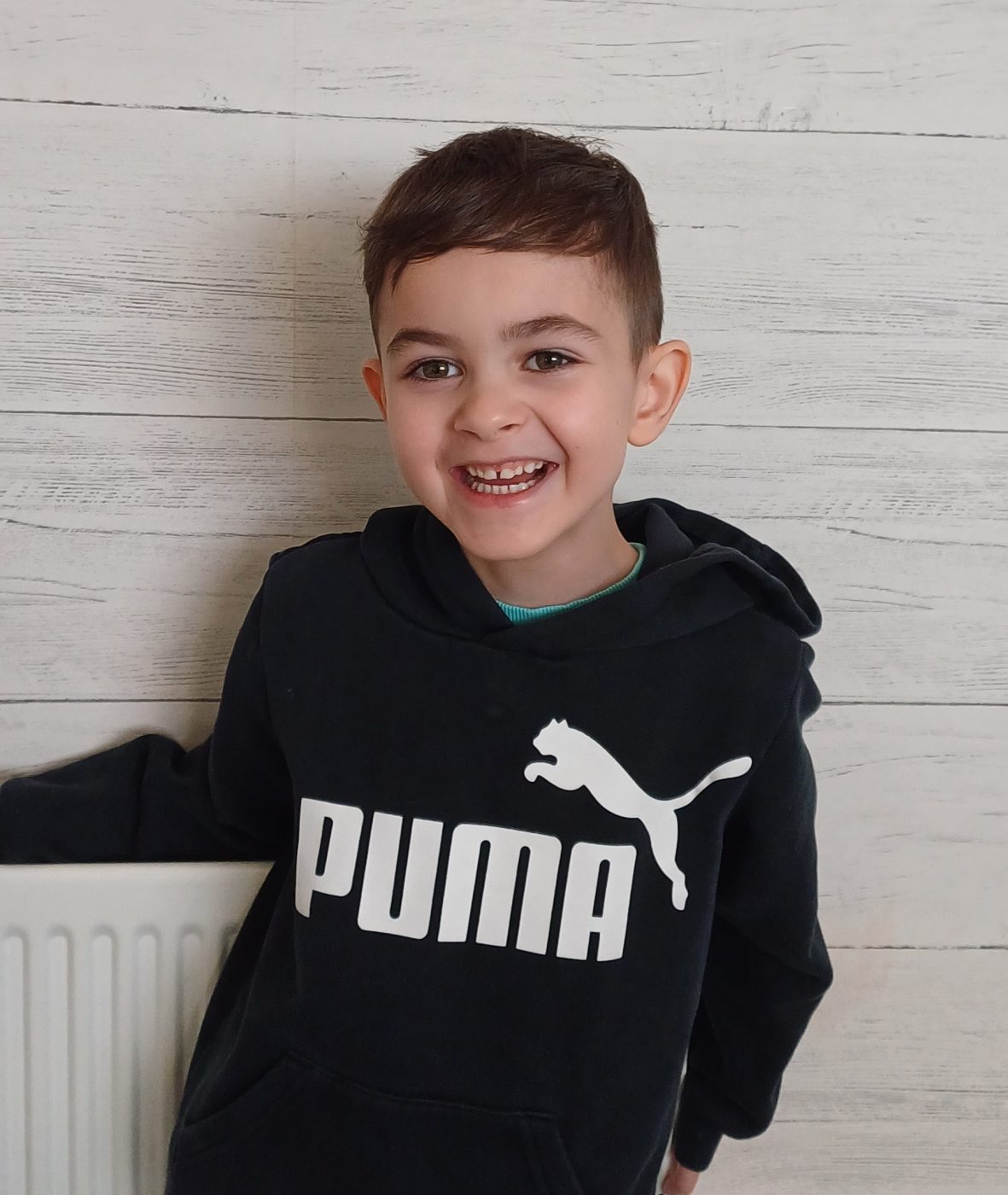
We’re delighted to announce that following Jude’s recent surgery that Jude is well, full of energy and ready for Christmas!
If you wish to donate any money to help the organisations who have helped Jude, please click here to see Judes JustGiving page.
The team at Redhill have some amazing charity events lined up for 2024 so watch this space!
Here is Jude’s story:
Jude is our rainbow baby, he also has a serious congenital heart defect – Double inlet left ventricle (DILV) and Transposition of the greater arteries (TGA).
DILV – In this single ventricle heart condition there is one large pumping chamber (ventricle) on the left side of the heart into which both collecting chambers (atria) empty their blood. This may affect the valves sitting in the middle of the heart. There is usually a large hole (ventricular septal defect) in the middle of the heart and a small pumping chamber (ventricle). The two major blood vessels leaving the heart, the pulmonary artery to the lungs and the aorta to the body, may leave from either the left or right sides of the ventricle and they may be swapped around (transposed). This means that a mixture of oxygen-filled and oxygen-empty blood passes to the lungs and to the body.
We received the devastating news at our 20-week anomaly scan, the sonographer was unable to view four chambers of the heart. We were referred to Birmingham Women’s Hospital to meet with the fetal cardiologist. After a detailed fetal cardiac ultrasound scan, we received our son’s diagnosis. The dedicated team of doctors and nurses were very sympathetic and comforting and informed us of the condition and the expectations of life for a child with a CHD. We decided without question to continue with our pregnancy and with the advice and support of the cardiology team, upon Jude’s arrival we would go for the palliative surgical path, unless supported comfort care was necessary, should surgery not be advised.
After regular antenatal appointments, an induction date was scheduled for 39 weeks gestation. Bags were packed and ready for birth and transfer to BCH.
Jude was born naturally (day before scheduled induction) on 14/05/18 @ 11:31pm, 6lb 10oz. Lovely and pink with SpO2 (oxygen in the blood) 99%. After 30 mins of skin-to-skin contact, he was taken to the neonatal ward. We were transferred to BCH at 3 days old.

Ward 11 – We met our amazing cardiology consultant Dr. Mike Harris.
First operation was at 2 weeks old (Jude was sleepy/tired, lowered SpO2, increased respiratory effort). A band was placed around the pulmonary artery to restrict the amount of blood flowing to the lungs. If lung vessels are left with too big a blood flow, this can damage them over time. After this operation, Jude was noticeably more awake and alert. We were home age 4 weeks.
Second operation, 9 months old – Open heart surgery. Bi-directional carvo-pulmonary shunt (Glenn shunt). SpO2 mid 80’s%. The aim for this operation is to redirect the blood flow of deoxygenated blood to the lungs by attaching the upper body vein (superior vena cava) directly onto the lung artery (pulmonary artery). We were home 4 days post op! Started Aspirin medication.
Third and final palliative operation, 5.5yrs – Open heart surgery.
Jude’s weight has always been a struggle! As he grew older the aim was to gain weight in preparation for his final surgery. We had regular support from the dietician at BCH.
Total carvo-pulmonary connection (Fontan completion). SpO2 77%, cyanosis, decreased energy levels.
This operation is to permanently separate deoxygenated and oxygenated blood supply. This increases the amount of deoxygenated blood to the lungs and improves the amount of oxygenated blood flow around the body.
Post operatively – Jude’s chest drains were all removed by day 4! This gave him the confidence needed to get up and move around the ward.
MCT diet – Medium chain triglycerides. After surgery and a further 4 weeks after removal of the chest drains, Jude needed to follow a strict MCT diet. He could only consume foods with 0.2g> of fat, with a daily exchange allowance of 4g per day. He managed this diet very well but is happy to be able to eat cheese again!
We were home 10 days post op, SpO2 93%!
Jude has now started his Warfarin journey. Due to having had open heart surgery and the risk of having a stroke/blood clot develop, Jude now takes daily Warfarin and will do so for the foreseeable future. We are currently having regular visits to BCH with the anticoagulation team to check his blood INR levels are within normal range. We hope sometime in the new year to be able to perform home INR testing, thanks to the generosity of the Young at Heart Charity, who will be gifting us with an INR machine.
Jude is thriving since having had his Fontan completion, he is benefiting so much and is full of energy. He had an amazing post op cardiac review, Dr Harris is very pleased with his recovery. Jude has also started his phase return to school, in time for all the Christmas activities.
We run a just giving page each year for Birmingham Children’s Hospital. This year we shared the donations between BCH and a charity called Pyjama Faries – Who are a volunteer based charity of seamstresses who make beautiful surgical pyjamas and gowns for children who will be visiting hospitals for operations or long stays.
Next year we will fundraise for Birmingham Children’s Hospital and the Young at Heart Charity, if you wish to donate to these amazing organisations please click here to see Judes JustGiving page.
Kim, Rob, Jonah and Jude Underhill